
reprinted from Exercise Is Medicine®, Australia
A large number of people are sedentary, and that number is increasing as more people worldwide are living in urban settings. Diseases of the developed world, such as cardiovascular disease and diabetes, are increasing worldwide at a rapid rate. indeed, the WHO states that chronic disease (i.e. noncommunicable disease) is now the major cause of death and disability worldwide. A handful of risk factors, including high cholesterol, hypertension, and obesity, cause the majority of chronic disease burden. A change in physical activity (PA) and exercise would have a major impact on eliminating these risk factors and reducing chronic disease.
Exercise is Medicine (EIM) calls upon health and medical practitioners to assess and review every patient’s physical activity program at every visit. But it is not enough to ask this of health and medical practitioners. We need to provide practical solutions in terms of implementing successful counselling and referral programs. An enormous amount of evidence shows that exercise improves overall health and advances the health of patients with chronic diseases. Working from this evidence base, we will show outcomes and discuss what we would like to see happen with EIM.
EIM complements other global and national initiatives that address the prevention of chronic disease and the promotion of physical activity and healthy lifestyles. Primary care strategies for physical activity are central to the WHO Action Plan for Preventing Chronic Disease, WHO Global Strategy for Diet, Physical Activity and Health, Federal Government’s Swap it program and Lifescripts, to name a few. By 2020, 80% of all deaths from chronic disease will be in developing countries (LMIC). The ability to effectively address this heavy disease burden will require effective strategies for PA and exercise promotion, especially within the primary care networks that form the core of the health care systems in most low – and middle-income countries (LMIC). EIM could be a key part of this shift in global health.
In 2010 Exercise & Sports Science Australia (ESSA) announced a Memorandum of Understanding with the American College of Sports Medicine (ACSM) to adapt and coordinate the Exercise is Medicine® initiative in Australia. Exercise is Medicine® Australia (EIM Australia) aims to combat the rising number of preventable disease and healthcare costs by establishing a national action plan through general practitioners, practice nurses and allied health providers, and via general population stakeholder engagement. Exercise is Medicine is asking our health and medical professionals to include an exercise prescription in all their treatment plans for patients. Years of research has highlighted the importance of exercise in the treatment and prevention of disease and the lowering of mortality rates. However, the majority of our health and medical professionals have failed to integrate exercise into the standard treatment of disease. Health and medical professions must start to encourage their patients to partake in regular physical activity, especially those with or those who are at risk of developing a chronic disease. If there was a pill available that had all the proven health benefits of physical activity and exercise, medical professionals would prescribe it regularly, all healthcare systems would ensure every patient had access to it and every patient would remember to take it. But there is not.
Thus, patients need to be advised to engage in 30 minutes of moderate exercise, such as a brisk walk, cycle or slow swim on most, or at least 5 days a week or 20 minutes of vigorous exercise, such as a run, on at least 3 days a week.
Why wouldn’t they when:
- Patients who attend a cardiac rehabilitation service have a 30% reduced risk of a second heart attack;
- On average, exercise reduces blood pressure by about 6–7 mmHg. Scientific studies have shown that, if systolic blood pressure is reduced by 5 mmHg, deaths from strokes decrease by 14% and deaths from coronary heart disease decrease by 9%;
- Strength and balance training has been shown to reduce the risk of falls by 40%; and
- People who already have T2DM can increase their fitness levels (and improve their symptoms) by about 12% through exercise training.
Thus, health and medical professionals should begin to use exercise as a medication to treat and prevent a variety of chronic diseases.
Evidence for physical activity and exercise interventions in primary care with a referral component
There are clear advantages to having GPs promote PA and exercise in their practices: large proportions of the population attend primary care each year, and patients see providers as credible sources of health advice and hence patients may be receptive to exercise information. The type of health care system in which a GP practices will strongly affect the kind of advice or PA/exercise intervention that they can deliver. For example, one must consider the reimbursement schedules for health and medical practitioners, especially for preventive counselling. In addition, PA/exercise advice in clinical settings may target prevention at several levels: primordial, primary, secondary, or tertiary prevention (see FIGURE 1).
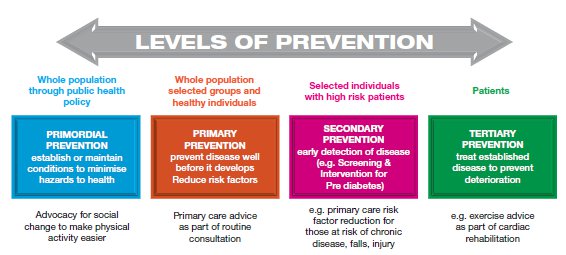
Exercise-promoting roles exist for practitioners across the prevention spectrum, beginning with advocating for preventive health (primordial prevention). Medical practitioners or practice nurses should ask about physical activity of all new patients (primary prevention), and especially among those at high risk of chronic disease (secondary prevention). Among those with established cardiovascular disease, diabetes, and many other chronic conditions, exercise prescription may be a beneficial component of therapy but will require medical clearance and ongoing support.
A review of PA/ Exercise interventions in primary care settings: Do they work?
The research literature on PA/exercise interventions has focused mainly on ‘brief advice’ interventions delivered by a GP, with far fewer studies on exercise referrals and community based programs. Hillsdon published a randomised controlled trial (RCT) in which he recruited 45 – to 64-year old sedentary adults in primary care. Patients were sent a questionnaire and randomised into one of three groups: those receiving direct advice, those experiencing a brief negotiation, and true controls. He found no significant difference in percent change in PA between interventions and controls at 12-month follow-up. Simons-Morton conducted a well-designed study in the US called The Activity Counselling Trial. He objectively measured how PA benefited cardiac fitness and found that two extended counselling protocols were better than advice alone in a primary care setting. Results persisted for 24 months. In another US study, entitled Patient- Centered Assessment and Counselling for Exercise and Nutrition (PACE), researchers looked at the effect of three conditions: advice/counselling by a physician;health education materials and exercise prescription; or follow-up phone call from a health educator. They validated their results using a Caltrac accelerometer. Results from the PACE study were not quite significant. A PACE study in the Netherlands that consisted of a RCT of 350 subjects found that both the intervention and control groups improved over time, but there was no significant difference between them. A study by Halbert et al. looked at the effect of an exercise specialist embedded within a clinical practice. In their study, an exercise specialist provided advice to patients with cardiovascular risk factors in an Australian general practice setting. They found this approach to be effective.
A study in the US examined the effect of a telephone counselling intervention. One GP in one family practice in Puget Sound participated. Inactive patients received three sessions of telephone counselling, 30 minutes each, from a health counsellor. The researchers found that the PACE score was higher in the intervention group, but that this difference was not significant.
In 2002, Smith et al. summarised all the literature on PA counselling in “Evidence for effectiveness of PA compared to other GP interventions.” They reported that smoking advice from a physician results in about 5% quit rates, alcohol advice yields approximately 10-14% quit rates, and nutrition advice results in a 5-8% change. PA advice yields about 10% change. These modest effects tend to be short-term, with limited evidence of longer-term effects. They concluded that investment in PA counselling in the primary care setting has the potential for population-level health gains.
Exercise is Medicine® Australia
Our mission for EIM Australia is:
- To make physical activity and exercise a standard part of a disease prevention and treatment medical paradigm in Australia; and
- For physical activity and exercise to be considered by all healthcare providers as a component of every patient visit, and that patients are effectively counselled and referred, as to their physical activity, exercise and health needs. Therefore leading to the overall improvement in the public’s health and long-term reduction in healthcare costs.
As a result of this project we expect to:
- Create broad awareness that physical activity and exercise is indeed medicine;
- Make “level of physical activity and exercise” a standard vital sign question in each patient visit (when appropriate);
- Help general practitioners and other health care providers to become consistently effective in counselling and referring patients as to their physical activity and exercise needs;
- Lead to policy changes in public and private sectors that support physical activity and exercise counselling and referrals in clinical settings;
- Produce an expectation among the public and patients that their health care providers should and will ask about and prescribe physical activity and exercise; and
- Appropriately encourage general practitioners and other health care providers to be physically active or engage in exercise themselves.
A key component of the EIM Australia program is the development of a website – www.exerciseismedicine.org.au which went live on 20th May 2011. This website comprises educational and support materials for general practitioners, practice nurses and allied health professionals to use in their practices. The website also includes information and links for the public, policy and advocacy groups, and the media.
Acknowledgement: EIM Global Roundtable reports
